Constipation – An in-depth Guide

As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
The word “constipation” is derived from the Latin words con (meaning “together”) and statis (meaning “to stand”) which together literally mean “to stop having bowel movements.” Constipation is a common ailment that affects nearly everyone at some point in their life but can be alleviated with simple lifestyle changes or medical intervention.
There are approximately 4 million people in the UK who suffer from constipation and an estimated 15 million people in the US. These figures double again for adults over the age of 60.
Many people suffer from constipation, which can significantly affect their quality of life. Here you can learn about who it affects, the symptoms, and how to diagnose and treat it.
We all know that constipation can be a painful and annoying condition, but did you realize it can also lead to more serious health problems?
That’s because when the colon isn’t emptying properly, toxins and waste products build up in the intestines.
This blocks the absorption of important nutrients from food and water. The build-up may also cause an infection called colitis or inflammatory bowel disease. These conditions could lead to weight loss, nausea, fever, and stomach pain.
Symptoms of constipation
Constipation is defined as having fewer than three bowel movements per week, despite the fact that everyone’s bowel movements are plainly different. It’s common to distinguish between two types of constipation:
- Acute constipation – is severe (described as situative or temporary)
- Chronic constipation – lasts a long time
Temporary constipation (situative) is not an illness, but a symptom, a sign from the body that something is wrong. Medically speaking, constipation is present when:
- There are less than three bowel movements a week
- They are accompanied by great effort and pressing
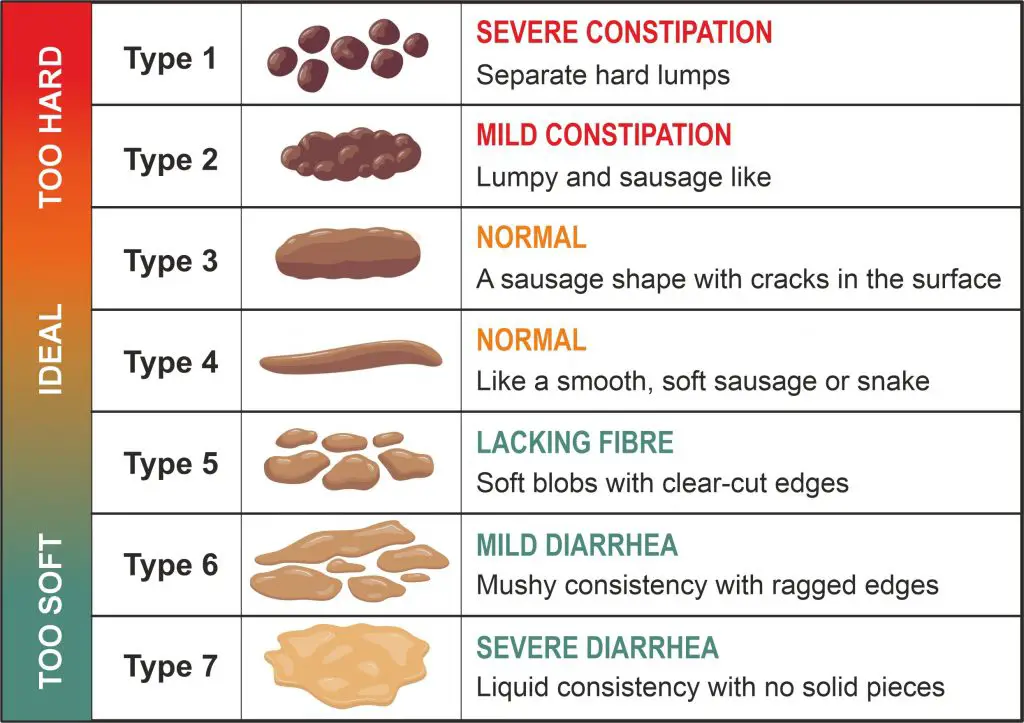
- Stools are hard and lumpy due to the long duration they have been in the bowels (see the Bristol stool form scale, type 1 and type 2)
- Symptoms located outside the bowels occur frequently
Acute constipation occurs quickly, usually within hours or days, but chronic constipation occurs over a prolonged length of time, frequently more than six months.
Chronic constipation is a state which has been present for at least three months and shows at least two of the following key symptoms at least in every fourth bowel movement:
Constipation is characterized by hard stools, pain during bowel motions, inadequate evacuation, and the sensation of a plugged rectum. If there is blood in the stools, severe abdominal aches, fever, or alternating constipation and diarrhea, visit a doctor as soon as possible.
- Stools are hard or lumpy (see the Bristol stool form scale, type 1 and type 2)
- The feeling of incomplete evacuation of the bowels
- The sensation of a plugged rectum, even after a bowel movement
- Straining or pain during bowel motions, especially with severe abdominal aches
- Pain within your lower back
- Trying to help evacuation with your hand
- Fewer than three bowel movements a week
- Passing lumpy, hard, or dry stools
- Blood within your stools
- Soft unshaped stools only when taking laxatives
- Irritable bowel syndrome has been excluded
As you can see in the diagram below, constipation is defined as Type 1 or Type 2 on the Bristol Stool Chart.
Who is primarily affected?
Constipation affects about one out of every four adults in the Western world. Constipation is a problem that affects and bothers a growing number of women, but it can also affect and bother parents of babies, small children, and children.
Certain people are more likely to become constipated, including2
- women, especially during pregnancy or after giving birth
- older adults
- non-Caucasians
- people who eat little to no fiber
- people who take certain medicines or dietary supplements
- people with certain health problems, including functional gastrointestinal disorders
Causes of constipation
The primary function of your colon is to absorb water from leftover food as it passes through your digestive system. It then makes a stool (waste).
The waste is eventually pushed out through the rectum and removed by the colon’s muscles. If the stool is left in the colon for an extended period of time, it can become hard and difficult to pass.
Constipation is a common side effect of a poor diet. To keep stools soft, eat a high-fiber diet and drink plenty of water.
Plant-based foods are typically high in fiber. Fiber comes in two types: soluble and insoluble. Soluble fiber dissolves in water and travels through the digestive system as a soft, gel-like substance.
As it passes through the digestive system, insoluble fiber keeps the majority of its structure. Stool absorbs both types of fiber, increasing its weight and bulk while softening it. This makes passing through the rectum easier.
Common causes of constipation include:
- A low fiber diet, particularly diets high in meat, milk, or cheese
- Dehydration
- Lack of physical activity
- Stress and psychological stresses
- Delaying the impulse to have a bowel movement
- Travel or other changes in routine
- Medication-related impairments, including certain antacids (heartburn remedies) containing calcium and aluminum, antidepressants, blood pressure drugs (beta-blockers), pain medications, diuretics, opiates (strong painkillers or cough medicine codeine), and more
- Piles, changes in the bowels, tears in the skin around the rectum (anal fissures), narrowing of the digestive tract, and other physical changes
- Reduced intestinal motility as a result of neurological conditions (e.g., multiple sclerosis, diabetes, Parkinson’s disease, and so on)
- Deficiency in electrolytes (e.g. a deficit of potassium, often also in the case of excessive use of laxatives)
- Hormone imbalance and metabolism impairment (e.g. thyroid underactive, diabetes, pregnancy)
- Older age (constipation affects around one-third of people ages 60 and over)
How constipation is diagnosed
Every diagnosis begins with a comprehensive examination of the patient’s medical history by a doctor. The doctor will discuss a number of topics with you.
- Organic bowel diseases that already exist
- Questions about various illnesses, such as Parkinson’s disease, multiple sclerosis, diabetic nerve problems (neuropathy), and so on.
- Questions about your ancestors (presence of illnesses in the family)
- The frequency of bowel movements, as well as the color and shape of the feces, are all factors to consider.
- Habits of eating and drinking
- Pain and flatulence are common side effects.
- Questions concerning the medication you’re taking and the effects it might have on your bowel movements.
- The thyroid gland’s function is examined.
Following the interview, the doctor performs a physical examination in which he examines the rectum and palpates and listens to the abdomen.
A stool sample can reveal digestive issues and the presence of incorrect bacteria in the intestines. In addition, blood that is not evident in the feces is checked (fecal occult blood).
A blood count is examined in the laboratory (thyroid gland hormones and electrolytes such as sodium, potassium, and calcium).
If these findings are normal, the patient is under 50, and no warning symptoms of functional constipation were discovered during the medical history interview (acute constipation, weight loss, blood in the stools, fatigue), treatment for functional constipation can begin.
In the case of chronic constipation, the examination will be more thorough, and the doctor may recommend a rectum and sigmoid colon proctoscopy, as well as a colonoscopy if there is a suspicion of large intestine disease.
Other ways to be diagnosed:
- Ultrasound examination of the entire abdomen is performed (sonography)
- Radiological examination of the bowels, which is now commonly done using computer tomography (CT)
- Establishment of the colon transit time (the duration until the food has passed through the bowels).
If an organic cause for constipation is discovered, the underlying condition must be addressed first. If there is no specific explanation for the sluggishness of the intestines that can be treated, general steps to alleviate constipation should be followed.

Relief and treatment from constipation
Changing your diet and increasing your physical activity level are the easiest and fastest ways to treat and prevent constipation.
Change of diet: foods high in fiber, such as wholemeal bread, dates, and brown rice, cause stools to expand and support good bowel function. It’s best to gradually increase the amount of fiber you consume, as an increase in symptoms (wind, abdominal pains, and a feeling of fullness) is to be expected until your intestines have adjusted.
Change your drinking habits: taking a glass of water before each meal helps to stimulate the bowels. Drinking a glass of cold water first thing in the morning on an empty stomach is especially useful. Limit consumption of alcohol and caffeinated drinks, which cause dehydration.
Exercise: is one of the keys to success when the bowels need to be stimulated, whether it’s cycling, swimming, jogging, or Nordic walking. Aim for about 150 minutes of moderate exercise every week, with a goal of 30 minutes per day at least five times per week.
Make it a habit to train your bowel movements. Suppressing a bowel movement is not a good idea! Retrain your bowels to go to the bathroom on a regular basis. Daily bowel movement training promotes a sense of regularity in your life.
Ways to stimulate bowel movements
Most people have a bowel movement once or twice a day. But some people have problems passing stools, and others don’t go at all. It is important to know the best way to stimulate these bowel movements so that your body can function properly.
There are many different methods you can try when it comes to stimulating bowel movements, from consuming prune juice in small doses throughout the day to taking magnesium supplements in order to relax the muscles of your intestines and rectum.
In addition, if you find yourself struggling with constipation due to certain medications or dietary restrictions, there are other treatments available depending on what is causing your problem – such as adjusting medication dosages or switching foods for ones high in fiber instead of low-fiber foods.
Try the following techniques to help you go to the toilet with more ease:
- If you feel the urge to have a bowel movement, don’t delay. The longer you wait, the harder your stool can become.
- When using the bathroom, allow yourself plenty of time, and try to relax your muscles.
- Raise your knees by putting your feet on a footstool when having a bowel movement.
- Massage the large intestine and complementary therapies: a five-minute clockwise abdominal massage along the large intestine stimulates the bowels.
- Breathing exercises along with yoga can strengthen the abdominal and pelvic floor muscles, as well as releasing and stretching the muscles of the legs, buttocks, and lower back, and massaging the connective tissue are all options (manual lymphatic drainage, foot reflex zone massage).
Ways to prevent constipation
Tips for preventing constipation are similar to those for relieving it.
Try the following:
- Eat plenty of fruits, vegetables, and whole grains.
- Eat high fiber foods and ask a healthcare professional about using fiber supplements.
- Include prunes or bran cereal in your diet.
- Drink plenty of water.
- Avoid alcohol and caffeine, as they can lead to dehydration.
- Get regular exercise.
- Consider adding probiotics to your diet, like those found in yogurt and kefir with live active cultures.
- Train your muscles to have a bowel movement at the same time each day.
In conclusion
We need a lot of probiotic bacteria in our intestines because they keep the process of breaking down food and making it available to the body going.
Fermentation and putrefaction processes begin when our gut flora is diminished and damaged (e.g., by medication (antibiotics), stress, or poor food), which can disrupt and slow down bowel function.
Probiotics with highly active bacteria strains are recommended for rebuilding and regenerating a damaged gut flora. They protect the mucosa of the intestine, improve metabolic activities, and can help you have more bowel movements.
A quick reminder ..
Probiotics.tips aim to provide the most up-to-date information, help, and advice for YOU to make informed decisions. If you are unsure or uncertain and require more clarity, please reach out to us and we will gladly come back and advise you as best we can.
The best means to reach us is via email at info@probiotics.tips or fill out the form on our Contact Us page – click here.
Probiotics.tips
About Us
Our goal is to empower you with concise probiotic guidance for a healthier gut. With expert advice, we provide the knowledge to improve your well-being and navigate the world of probiotics efficiently, ensuring you achieve optimal gut health.
- Can You Take Probiotics While Water Fasting?
- Does Fasting Help Microbiome Diversity and Functionality?
- Does Fasting Help Your Bowels
- Does Fasting Help Probiotics? Understanding Gut Health Benefits
- Does Fasting Help the Gut: Understanding the Impact on Digestive Health
Disclaimer
As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
Check these out on Amazon








