Taking Probiotics with Antibiotics – A Concise Guide
As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
Probiotics are important for gut health and many people take them to improve their digestion, but did you know that you should also take probiotics when you’re taking antibiotics?
Antibiotics can kill the good bacteria in your gut, which can lead to digestive problems.
Taking probiotics with antibiotics helps to replace the good bacteria that was killed by the antibiotics and it can help to prevent diarrhea and other digestive problems.
According to a study published in the journal “Microbiology,” taking probiotics with antibiotics may help reduce the risk of developing antibiotic-associated diarrhea by up to 60%.
National Library of Medicine
Antibiotics and gut health
Antibiotics, without a question, serve a critical function in modern medicine in preventing and treating bacterial infections. Bacterial infections are no longer the leading cause of death in the modern world, thanks to antibiotics. Antibiotics, on the other hand, have recently been shown to have a deleterious impact on our gut microbiome.
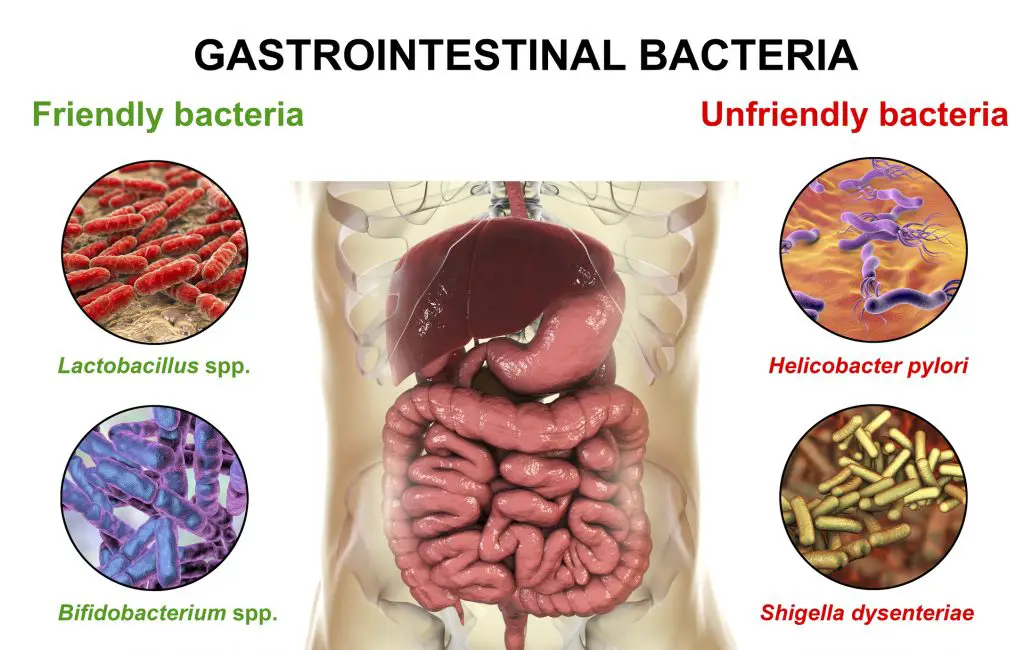
The gut microbiome is a sophisticated ecology of billions of microbes that coexist in our gastrointestinal tract in perfect harmony. These microorganisms have a wide range of health benefits, including improved digestion, immunity, skin health, and vitality. Beneficial microorganisms must coexist with more dangerous microbes that normally colonize the gut. Various lifestyle factors, such as a low-fiber diet, travel, and infection, can all disrupt this equilibrium.
So, when we take an antibiotic, what happens to our gut microbiome? Antibiotics, unfortunately, can be harmful to our gut health. Antibiotics, while effective in killing bad bacteria, are fundamentally non-selective and can reduce good bacteria in the stomach.
When taking an antibiotic, this is thought to lead to the development of diarrhea, constipation, and/or vaginal thrush. This change to our gut microbiome can lead to an overgrowth of harmful bacteria like Clostridium difficile in some situations.
Of course, in cases of active infection, the advantages of antibiotics far outweigh the risks. Taking probiotics with antibiotics can help to reduce the stomach discomfort caused by a shift in our gut flora, also known as dysbiosis.
What are the most common side effects of probiotics?
The most common side effects reported with probiotics in clinical trials included:
- Abdominal bloating
- Abdominal pain
- Appetite loss
- Chest pain
- Constipation
- Diarrhea caused by antibiotics
- Fatigue, a lack of energy, or a feeling of being ‘wiped out’
- Flatulence
- Gas
- Increased phlegm
- Indigestion
- Nausea
- Rash
- Taste disturbance
- Vomiting
Why taking probiotics with antibiotics is wise?
Following antibiotic use, replenishing the gut microbiome with probiotics aids in rebalancing the gut microbiome. The benefits of probiotic supplementation have been recognized by the NHS. When prescribed antibiotics, many people now opt to take a probiotic supplement to complement their natural flora. When prescribing antibiotics, your pharmacist may even suggest probiotics.
Antibiotic-associated diarrhoea (ADD) is one of the most prevalent antibiotic side effects, with an incidence ranging from 5 to 35 percent, depending on the antibiotic used. In 2012, a meta-analysis of 23 trials (focused on contrasting and integrating results from numerous studies) found that taking probiotics with antibiotics could help with antibiotic-associated diarrhea. Clostridium difficile infection is one type of AAD that causes chronic diarrhea and, in severe cases, colitis.
This is especially concerning in the elderly, and it can be fatal in some cases. Evidence suggests that taking probiotics with antibiotics is both safe and effective in helping to support the health of the gut microbiome and reducing digestive upset related to Clostridium difficile-associated diarrhea, according to a systematic review and meta-analysis of 23 randomized controlled trials involving 4213 patients. Health professionals can learn more about probiotics and Clostridium difficile by visiting this page on the Professionals site.
Can I take probiotics with antibiotics?
Yes. According to extensive clinical research, the best probiotics to take with antibiotics are specific strains that can be given together rather than separately. Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, and Bifidobacterium lactis Lafti B94 are the strains in question. Most other probiotic supplements cannot be taken at the same time as antibiotic medicine, which is not the case with these strains.
Taking different probiotic strains with antibiotic medicine isn’t always negative or counterproductive; it merely means that the probiotic might not be viable, but the antibiotic medication won’t be harmed. Because not all probiotics are created equal, it’s always a good idea to take strains of probiotics that have been tested to help with the health condition or scenario you’re trying to support.
Taking well-studied strains that have been proved to survive when taken at the same time as the antibiotic prescription is especially beneficial when using intravenous (IV) antibiotics, which are often given on a continuous drip. We always recommend taking probiotics with antibiotics throughout and after any antibiotic treatments.
Which are the best probiotics to take alongside antibiotics?
A common question we hear a lot is, “What are the best probiotics to take with antibiotics in terms of diarrhea?” As can be seen from the examples above, it appears that this is the primary cause for concern when taking this type of medication.
When taking probiotics with antibiotics, it’s critical to choose strains that have been evaluated in clinical studies and have been shown to reach the stomach alive. The more friendly bacteria in your gut, the less likely you are to suffer digestive problems like diarrhea.
Three probiotic strains have been found to achieve this.
- Lactobacillus acidophilus Rosell-52
- Lactobacillus rhamnosus Rosell-11
- Bifidobacterium lactis Lafti B94
They can be taken at the same time as antibiotics without causing any problems. This is how a supplement containing this probiotic combination should be used:
- Even if you’re on antibiotics, take one capsule with breakfast every day.
- Take once a day for the duration of the antibiotic course, and preferably for one week afterward.
- Continue until the pack is finished, and if the antibiotic treatment lasts longer than one week, add a second pack.
Clinical trials around taking probiotics with antibiotics
Participants were given Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, and Bifidobacterium lactis Lafti B94 alongside antibiotics in clinical studies for Helicobacter pylori infection; all three cultures were demonstrated to thrive alongside the medication.
Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, and Bifidobacterium lactis Lafti B94, which have been tested in this age range, can also be given to children aged 1 year and higher. Parents may want to look for a supplement designed specifically for children’s digestive health.
For those with a vaginal infection who are taking antibiotics for an intimate health problem, probiotic strains such as Lactobacillus reuteri RC-14® and Lactobacillus rhamnosus GR-1® may be worth exploring. These strains are frequently used in conjunction with antibiotics for vaginal infections, although they should be given at least 2 hours apart.
Do antibiotics kill probiotics?
Only a few probiotic strains have been found to survive when taken concurrently with antibiotics. Because all antibiotics have some sort of detrimental effect on the gut microbiome, it’s critical to choose the optimum probiotic strains when taking this type of medication.
You want strains that have been studied not only for their ability to survive when taken alongside antibiotics but also for their ability to provide benefits.
The comprehensive analysis behind the three Lactobacillus strains listed above distinguishes them from many other probiotic supplements on the market today, making them a good alternative for anyone who wants to take natural bacteria while on antibiotics. Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, and Bifidobacterium lactis Lafti B94 have also been examined and found to tolerate stomach acidity and bile salts in vitro.
When should I take probiotics when taking antibiotics?
With a few exceptions, we recommend taking your probiotic pills with breakfast in the morning. If you’re taking antibiotics plus a probiotic with the strains Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, or Bifidobacterium lactis Lafti B94, you can still follow this advice and take both with your breakfast.
If you’re taking many strains, though, it’s advisable to wait two hours between taking antibiotics and taking the probiotic supplement. So, if your doctor has directed you to take your antibiotics with breakfast, you would take the antibiotics first and wait two hours before taking the other probiotics. It’s best to take dietary vitamins with meals, such as with lunch or a mid-morning snack in this situation.
Alternative probiotic strains should, ideally, have evidence confirming their benefit under antibiotic treatment. If you’re taking a probiotic from a different company, you should ask them about the time you should wait between taking their product and taking your antibiotics.
Many firms advocate waiting 1 or 2 hours after taking antibiotics before taking probiotics as a general rule. Sufficient levels of helpful bacteria are able to reach the gut alive after this period of time. Taking probiotics every day while on antibiotics is generally recommended; this way, you may replenish your friendly bacteria on a daily basis before your digestive system is affected by a long-term microbial imbalance.
How should I take probiotics with antibiotics?
If you opt to take a probiotic with an antibiotic, start it on the same day as the medication, but not at the same time. After taking your antibiotic, wait at least two hours before taking your probiotic.
On an empty stomach, probiotics are normally taken twice a day. They should be continued for at least a few weeks after your antibiotic treatment is ended, though some people take probiotics on a daily basis to not only aid digestion but also to boost their immune system and improve nutritional absorption.
If you want to take probiotic supplements, look for a high-quality probiotic from a reputable brand that contains at least one of the following strains at 5 to 40 billion colony units per day: Lactobacillus rhamnosus, Saccharomyces boulardii, or Bifidobacterium sp.

What are the best probiotics to take after antibiotics?
Even if you took a probiotic designed to be taken with antibiotics, it’s always a good idea to take a strong daily probiotic for at least a month or two following antibiotics to rebuild your gut microbiota.
Scientists are unsure how long it will take to rebuild the gut flora after antibiotics; as it will rely on a variety of factors, including the individual’s gut microbiota, the length of the treatment, the strength of the medication, diet, and lifestyle, and so on. So, following antibiotics, what are the best probiotics?
After antibiotics, taking a probiotic supplement containing the Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07® strains may assist to stabilise Lactobacillus populations in the gut, according to research. The Lactobacillus genus of friendly bacteria helps to maintain our gut environment healthy by crowding out the bad guys.
Best probiotics for long-term antibiotic use?
If you’re on a long course of antibiotics, it’s a good idea to check for studies on the best probiotics. If you need to take antibiotics for a long time, you might want to look for a supplement that contains Lactobacillus acidophilus NCFM®. When taken alongside antibiotics, a supplement containing this strain has been shown in a randomized controlled experiment to reduce disruption to the gut microbiota composition.
When antibiotics are taken for more than two weeks, this can be beneficial. It is recommended, however, that this probiotic strain be taken 2 hours apart from an antibiotic rather than at the same time.
Do probiotics disturb antibiotic functioning?
There is no evidence that probiotics interact with antibiotic action in any manner, according to current research. Probiotic supplements and probiotic foods, such as yogurts or kefir, are now frequently recommended by doctors and GPs to be taken alongside antibiotics.
A study done in 2017 by the Department of Experimental Medicine at the University of Copenhagen in Denmark found out how probiotic therapy can affect antibiotic treatment.
The study was designed to see if it would be possible for bacteria from the gut microbiota to influence the efficacy of antibiotics for skin infections. It is well known that antibiotics are ineffective against infection when there is no improvement after one week, so they stopped giving them after 7 days. But this experiment showed that with or without taking probiotics, most patients got better within 8 weeks and were able to stop using antibiotics.
The conclusion was that neither group had any benefit over the other but both groups improved equally fast with their skin infections. They found out that taking probiotics didn’t affect the ability of antibiotics to fight bacteria in the skin infection, however, this doesn’t mean that we should stop using probiotics when we’re on antibiotics.
We still need to take them because they help your immune system and digestive tract function well and help you recover faster and feel better.
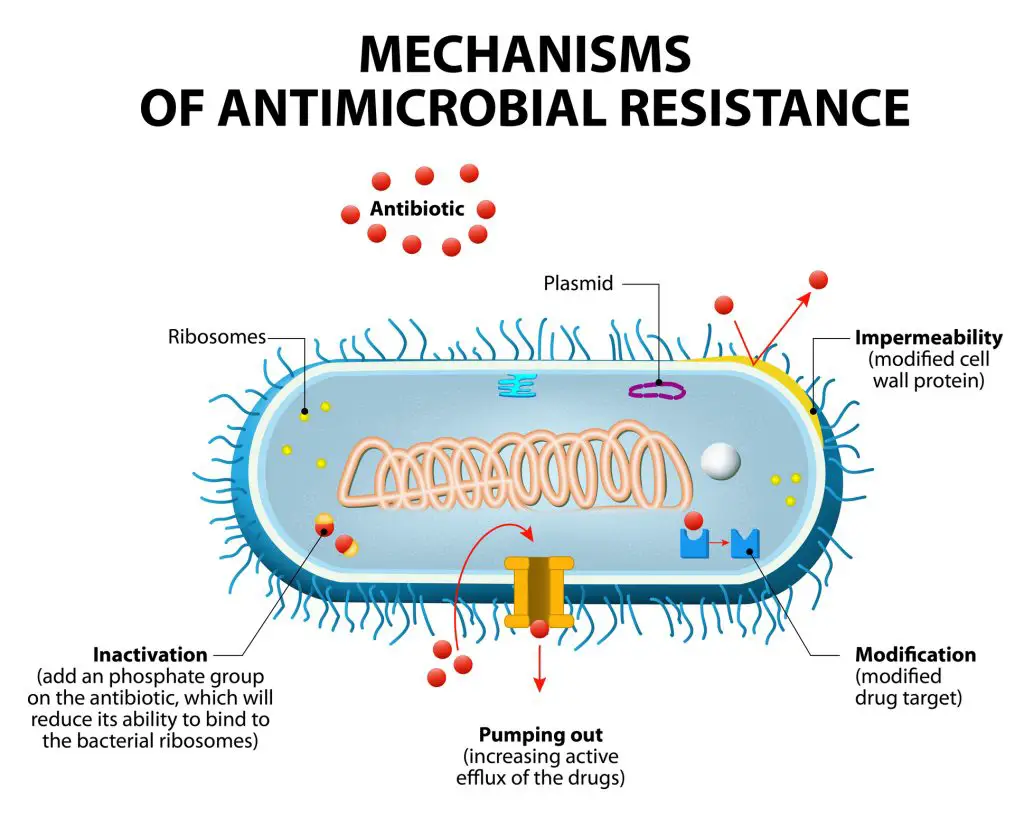
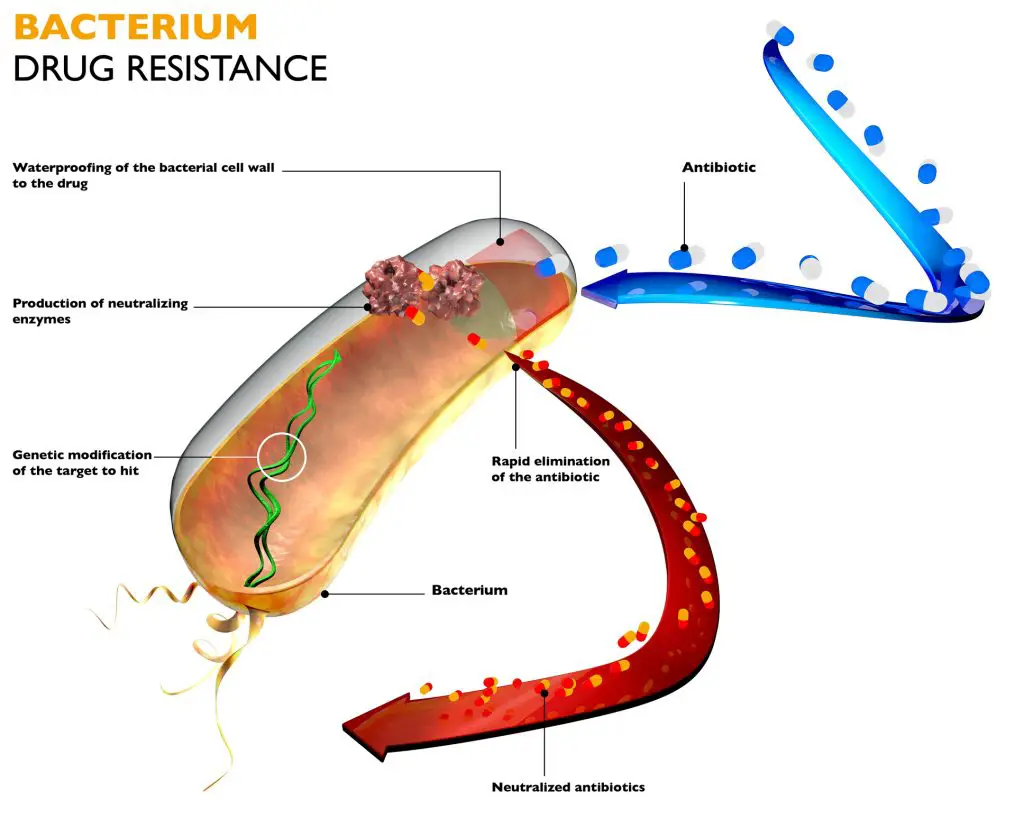
Over-prescription of antibiotics and antibiotic resistance
Antibiotic resistance is becoming a major public health concern. The World Health Organization (WHO) released a report that analyzed data from 114 nations and labeled antibiotic resistance as a “serious global issue.” They claim that basic, common diseases that aren’t considered life-threatening today could become killers in the future due to antibiotic resistance.
As a result, actions must be done to prevent the spread of antibiotic resistance and change how antibiotics are used and prescribed. Antibiotic overuse and prescription are key contributors to the development of antibiotic resistance.
Antibiotic overuse is a serious problem in the United Kingdom, with the NHS deeming up to 23% of antibiotic prescriptions “inappropriate”. More information about antibiotic overuse for healthcare professionals can be found here.
Antibiotic resistance is thought to be exacerbated by not finishing a full course of antibiotics. Probiotics are increasingly being utilized to aid digestion while taking antibiotics, potentially allowing patients to finish their treatment. More information on the use of probiotics to combat antibiotic resistance may be of interest to health professionals.
The lack of consistency in the findings on probiotics comes in part because they are being treated like conventional drugs.
Do prebiotics help return the gut microbiome to normal?
Prebiotics are fiber-rich foods including fruits, vegetables, and grains that feed probiotic bacteria.
Although there is no scientific evidence to support this, combining prebiotics and probiotics, such as yogurt with fruit and cereal or sauerkraut with a vegetable stir fry, may well be beneficial to your stomach.
Vegetables such as artichokes, asparagus, garlic, onions, and any green vegetable; fruits such as bananas, berries, and tomatoes; herbs such as chicory or garlic; grains such as barley, oat, and wheat; and other fibers such as inulin, which can be purchased separately or added to granola bars, cereal, and yogurt are all good prebiotic foods.
Important tips for supporting general health whilst taking antibiotics
- Consume foods that have been fermented or that contain prebiotics. After treatment of antibiotics, they can help reset the gut microbiota and improve gut health.
- Avoid refined sugary foods, since they feed the dangerous bacteria and yeasts that often grow out of control as a result of antibiotic use.
- Even if your antibiotics aren’t contraindicated, stay away from alcohol. Alcohol can also affect the gut microbiome and impair immunological function, making it more difficult for your body to fight infection.
- Make sure you finish your antibiotic treatment. Antibiotics might be difficult to keep taking due to unpleasant side effects, yet failing to finish the course increases the chance of antibiotic resistance.
- Maintain a balanced diet. Don’t rely solely on antibiotics; include a variety of immune-boosting foods, such as citrus fruits and green leafy vegetables that are high in vitamin C and other antioxidants.
Probiotics and antibiotics: a quick overview
- Antibiotics diminish the colonies of friendly bacteria in the gut, which can lead to digestive problems, therefore choosing probiotics to take with antibiotics is critical; don’t wait until the course is completed.
- Take Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11, or Bifidobacterium lactis Lafti B94 with breakfast if you’re taking them. If your antibiotic is also taken at breakfast, these strains can be taken at the same time.
- If you’re taking a different probiotic supplement, wait at least 2 hours after you’ve finished your antibiotics.
- It is critical to always follow your doctor’s recommendations and to take and finish an antibiotic treatment as directed. Taking probiotics with antibiotics can help with digestion and allow you to finish the course, lowering the risk of antibiotic resistance.
- If you’ve already finished a course of antibiotics and haven’t been advised to take a probiotic, it’s better late than never; take a probiotic now! You’ll be able to take them both during and after the next time.
- It’s not a choice between antibiotics and probiotics; it’s an option of taking antibiotics and probiotics together.
In conclusion
When you take antibiotics, it’s important to also take probiotics. Probiotics are the healthy bacteria that live in your gut and help keep your digestive system working properly. Antibiotics can kill these bacteria, which is why taking probiotics with them helps restore balance to your intestinal tract after antibiotic treatment.
There are many types of probiotic supplements available on the market today, but be sure that whatever supplement you choose has at least 1 billion CFUs (colony forming units) per capsule or tablet. This will ensure that there is enough active culture for all of the good bacteria in your gut.
As a result, identifying and personalizing a probiotic treatment to work on something as complex and unique as your own internal ecosystem is a difficult undertaking. With this in mind, it’s not unexpected that a dried-up pack of bacteria from the grocery shelf might not be sufficient.
Taking probiotics with antibiotics FAQs
Below we have a list of some commonly asked questions in regards to taking probiotics with antibiotics.
Are probiotics an alternative to antibiotics?
Alternatives to antibiotics are certainly worth investigating, but in the case of a bacterial infection, this should ideally be done under the guidance of a healthcare professional. Antibiotics are not always required; for example, in the event of viral illnesses, antibiotics will be useless (because antibiotics, by nature, target bacteria). There are also a variety of mild bacterial illnesses that can be treated without the use of antibiotics. It’s worth noting that up to 42% of uncomplicated urinary tract infections can clear up on their own in 48 hours, especially when given plenty of water.
Should I choose between a probiotic or an antibiotic?
The question of whether a probiotic or an antibiotic should be taken is frequently asked. In a nutshell, the answer is that it isn’t an either/or situation! Instead, the question is whether a probiotic should be taken instead of, or in addition to, an antibiotic. In the vast majority of circumstances, the answer is yes!
Can antibiotics cause diarrhea?
Antibiotic therapy can cause diarrhea, which is known as antibiotic-induced diarrhea or antibiotic-associated diarrhea.
Antibiotics kill both healthy and bad bacteria in the gut, disrupting the usual balance of microorganisms in the intestines.
Until the antibiotic therapy is finished, a minor incidence of soft stools or diarrhea is common. Colitis, colon inflammation, and infection caused by Clostridium difficile, is a more significant side effect of antibiotic-induced diarrhea (C. difficile).
Severe, watery diarrhea, stomach cramps and discomfort, fever, weight loss, and pus or blood in your feces are all possible side symptoms of C. difficile. If you have C. difficile symptoms, see your doctor right once for an evaluation and treatment.
When taking antibiotics when should I take probiotics?
Many brands advocate waiting 1 or 2 hours after taking antibiotics before taking probiotics as a general rule. Sufficient levels of helpful bacteria are able to reach the gut alive after this period of time.
What happens if you take a probiotic with an antibiotic?
Taking probiotics during and after an antibiotic course can help lower the risk of diarrhea and restore the health of your gut microbiota. Furthermore, after taking antibiotics, eating high-fiber foods, fermented foods, and prebiotic foods may help rebuild a healthy gut microbiota.
A quick reminder ..
Probiotics.tips aim to provide the most up-to-date information, help, and advice for YOU to make informed decisions. If you are unsure or uncertain and require more clarity, please reach out to us and we will gladly come back and advise you as best we can.
The best means to reach us is via email at info@probiotics.tips or fill out the form on our Contact Us page – click here.
Probiotics.tips
About Us
Our goal is to empower you with concise probiotic guidance for a healthier gut. With expert advice, we provide the knowledge to improve your well-being and navigate the world of probiotics efficiently, ensuring you achieve optimal gut health.
- Can You Take Probiotics While Water Fasting?
- Does Fasting Help Microbiome Diversity and Functionality?
- Does Fasting Help Your Bowels
- Does Fasting Help Probiotics? Understanding Gut Health Benefits
- Does Fasting Help the Gut: Understanding the Impact on Digestive Health
Disclaimer
As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
Check these out on Amazon








