Is Intermittent Fasting Good for Gut Microbiome?
As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
Integrating periods of fasting into your routine might seem like just another health trend, but its effects on your body, particularly the gut microbiome, are being studied with keen interest. Intermittent fasting, which includes cycles of eating and not eating, is increasingly recognised for its potential impact on health. Research suggests that one of the benefits of this eating pattern could be related to the diversity and function of the gut microbiome, the community of microorganisms living in the digestive tract that plays a critical role in overall health.
The relationship between intermittent fasting and the gut microbiota is multi-faceted, involving changes in the composition and activity of these microbes. While the gut microbiome is implicated in numerous health aspects, including digestion, immune function, and even mood, the idea that modifying eating patterns could influence this complex system offers an intriguing avenue for improving health. Scientific investigations have revealed that intermittent fasting may indeed promote a positive restructuring of the gut microbiota, potentially contributing to improved metabolic outcomes and protection against various diseases.
Key Takeaways
- Intermittent fasting has been linked to positive changes in gut microbiota.
- The diversity of the gut microbiome may be enhanced through fasting cycles.
- Health improvements may be tied to the altered gut microbial community in fasters.
Understanding Intermittent Fasting
Intermittent fasting (IF) is a dietary approach where you oscillate between periods of eating and fasting, which can lead to various health benefits, including improvements to your gut microbiome.
Types of Intermittent Fasting Regimens
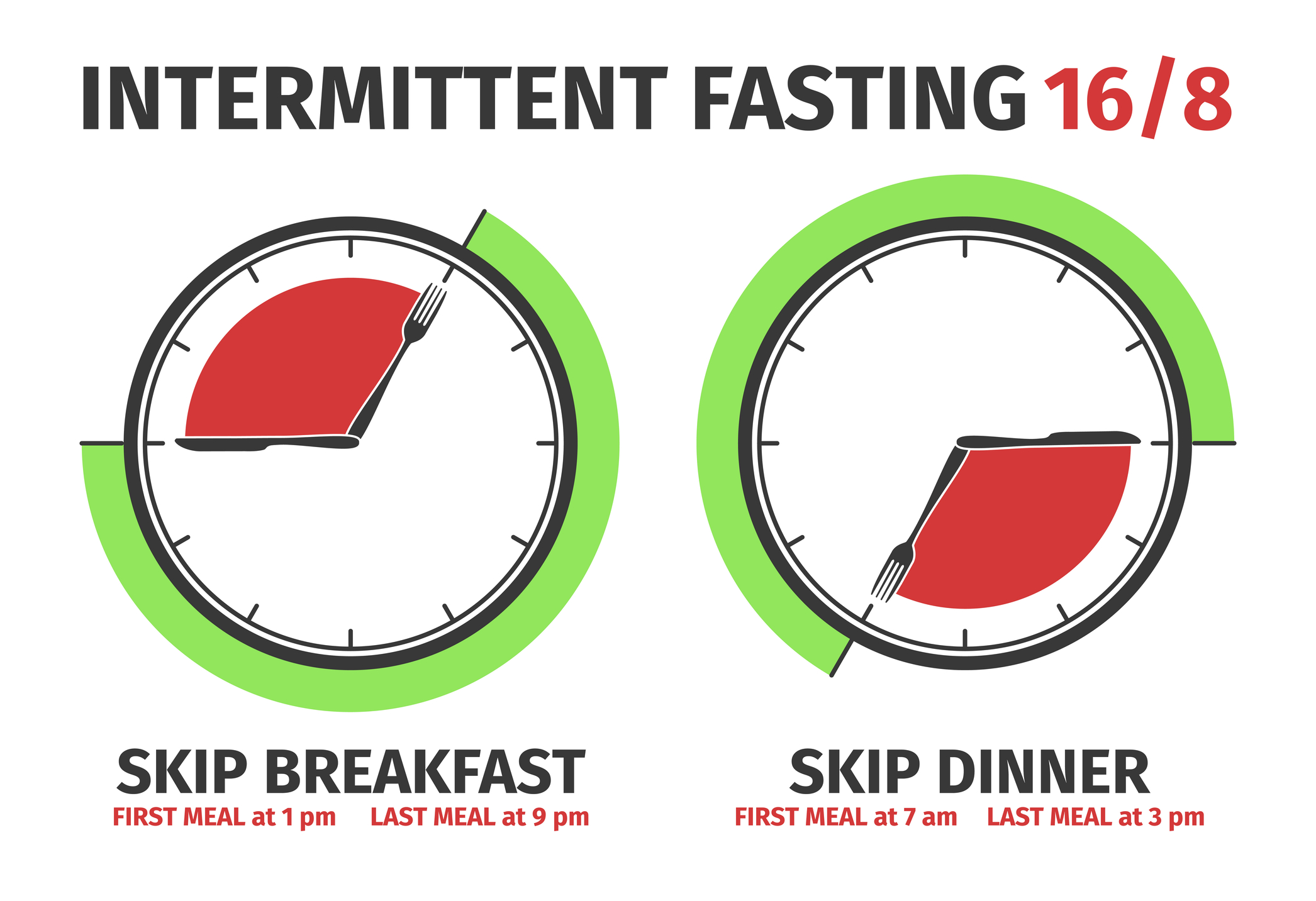
Time-Restricted Feeding (TRF): This regimen, such as the 16/8 method, confines your daily eating window to 8 hours, followed by a 16-hour fast. Alternate-Day Fasting (ADF): Involves alternating days of normal eating with days where you either fast or consume a significantly reduced calorie intake. Daily Fasting: This involves a consistent, shorter fast every day, typically for about 12 to 20 hours. Ramadan Fasting: A form of religious fast during the Islamic holy month of Ramadan, where you refrain from eating and drinking from dawn to sunset.
Historical and Cultural Practices of Fasting
Fasting has been practised for millennia across various cultures and religions. Notably, Islamic fasting during Ramadan is a form of ADF where individuals fast from dawn to dusk, abstaining from food and drink, which may influence metabolic health. Intermittent fasting in various forms is also evident in other cultural practices.
Physiological Effects of Intermittent Fasting
Fasting exerts its effects by tapping into your metabolism to use stored energy, potentially leading to improved blood pressure and body weight management. Engaging in intermittent fasting may align with your circadian rhythms, which can impact your overall metabolic health and energy levels.
The Gut Microbiome and Its Role in Health
The gut microbiome consists of trillions of microorganisms which play a crucial part in your overall well-being, affecting everything from metabolic processes to immune system regulation.
Composition and Function of the Gut Microbiota
Your gut microbiota is a complex and diverse ecosystem made up of bacteria, viruses, fungi, and other microscopic living things. Each organism has a role, from digesting food to synthesising vitamins and regulating the immune system. The composition of your gut microbiota is unique to you and can be affected by factors such as diet, lifestyle, and medications.
Microbiota Diversity and Its Importance
Microbial diversity in the gut is an indicator of gut health. Higher alpha diversity, which refers to the variety of microbes within your own system, is linked to a robust gut. On the other hand, beta diversity, describing differences between individuals, can give insights into population-wide health trends. Balanced microbial diversity is essential for maintaining the gut barrier and preventing pathogens from causing harm.
Dysbiosis and Related Health Disorders
Dysbiosis is an imbalance in your gut microbial composition, often resulting in adverse health effects. Conditions such as obesity, type 2 diabetes, cardiovascular disease, hypertension, and inflammatory bowel disease have all been associated with dysbiosis. Restoring balance to your gut microbiota is becoming a target for treating and possibly preventing these disorders.
Intermittent Fasting and the Gut Microbiome
Intermittent fasting (IF) has emerged as a lifestyle choice with potential benefits for your gut microbiome, impacting its composition, specific bacterial populations, and associated health markers.
Influence on Microbiota Composition and Diversity
Engaging in intermittent fasting can revamp the diversity and composition of your gut microbiota. Studies have demonstrated that during periods of fasting, the overall microbial richness increases, which is a positive marker for gut health. This rise in richness implies a greater variety of bacterial species in your gut, which is believed to enhance gut resilience against disturbances and support overall health.
Impact on Specific Microbial Species
The practice of intermittent fasting selectively increases populations of beneficial bacteria such as Akkermansia, Faecalibacterium, and Bacteroides. These specific bacteria have been associated with positive health outcomes. For instance, Akkermansia is known for its role in strengthening the gut barrier and has been inversely linked with obesity and metabolic syndrome. Similarly, Faecalibacterium prausnitzii—a major producer of the short-chain fatty acid butyrate, is renowned for its anti-inflammatory properties.
Effects on Metabolic and Inflammatory Markers
Intermittent fasting can influence various metabolic and inflammatory markers within your body. Fasting periods have been linked to reductions in C-reactive protein (CRP), an inflammatory biomarker, and improvements in insulin resistance. Additionally, changes in the gut microbiota during fasting contribute to the increased production of short-chain fatty acids such as butyrate, propionate, and acetate. These metabolites play critical roles in maintaining gut lining integrity, providing energy to colon cells, and modulating the immune system, which could indirectly help in managing inflammation and metabolic health.
Health Outcomes Associated with Intermittent Fasting
Intermittent fasting (IF) has been linked to various health benefits, particularly related to digestive health, weight management, and overall metabolic well-being.
Weight Management and Obesity
Intermittent fasting can contribute to weight loss and help in the management of obesity. It does so by creating periods where your caloric intake is markedly reduced, which can lead to a decrease in body weight. Studies show that IF may reduce adipose tissue, more commonly known as body fat, which is crucial for reducing BMI and improving health outcomes.
Improvements in Metabolic Disorders
For those contending with metabolic syndrome or type 2 diabetes, intermittent fasting may offer improvements by regulating blood sugar levels and increasing insulin sensitivity. This approach to eating can also positively affect various markers of metabolic health, such as serum triglycerides, LDL cholesterol (often referred to as ‘bad cholesterol’), and boost HDL cholesterol (the ‘good’ cholesterol).
Cardiovascular Health and Disease
The impact of IF on cardiovascular diseases is noteworthy. Regular fasting can lead to better heart health by managing blood pressure and reducing the risk of hypertension, a significant risk factor for cardiovascular disease. With a reduction in risk factors like high LDL cholesterol and body weight, your cardiovascular health may benefit from intermittent fasting.
Research and Evidence on Intermittent Fasting and Microbiota
In the pursuit of understanding the effects of intermittent fasting on gut microbiota, various studies have shed light on its potential impacts. Your knowledge of these effects is informed by human clinical trials, animal model research, and systematic reviews of the collected evidence.
Human Studies and Clinical Trials
Recent clinical trials on humans have begun to uncover the various ways that intermittent fasting may influence your gut microbiome. Specifically, a systematic review published on PubMed examined the effects of intermittent fasting on human volunteers and suggested alterations in the composition of gut bacteria, particularly an increase in Akkermansia muciniphila, which is associated with improved metabolic health. Another study found that these changes in the gut microbiota might revert to baseline upon resuming a normal diet, indicating a potential for gut microbiome resilience.
Animal Model Research
Research involving animal models, such as mice, has provided insights into the mechanisms by which intermittent fasting might benefit your gut microbiota. Findings suggest that fasting can promote white adipose browning—a process beneficial for weight management—and enhance gut barrier function, largely influenced by the presence and activities of certain gut microbial species. These studies are supportive of the hypothesis that intermittent fasting can favourably modify the gut environment in ways that may be beneficial for health.
Systematic Reviews and Meta-Analyses
Comprehensive systematic reviews and meta-analyses have been conducted to collate data from various studies. These reviews, which can be accessed via PubMed, evaluate the consilience of evidence from both human and animal studies. The overarching narrative from these analyses establishes intermittent fasting as a modifier of gut microbiota composition, with the potential to influence overall health positively. However, the reviews also call for more randomised controlled trials to substantiate initial findings and provide a clearer picture of the long-term consequences of intermittent fasting on the gut microbiome.
Lifestyle Considerations and Practical Applications
Making lifestyle modifications through intermittent fasting involves understanding the timing and quality of your meals as well as their interaction with exercise. It’s about fitting fasting into your routine in a healthy and sustainable way.
Integrating Intermittent Fasting into Daily Life
To successfully incorporate intermittent fasting into your life, it’s pivotal to tailor the eating approach to your daily schedule. Time-restricted feeding is a popular method where you eat all your meals within a specific window, typically 8-10 hours of the day. For example, consuming your meals between 12 pm and 8 pm aligns with many people’s lifestyles, helping to maintain consistency. It’s crucial to consider your typical day, work hours, and family commitments when determining your feeding window to ensure adherence and minimise the impact on your social life.
Nutritional Considerations and Diet Quality
While intermittent fasting focuses primarily on meal frequency and timing, the quality of your diet should not be compromised. It’s essential to consume a healthy diet rich in nutrients during your eating periods. Prioritise whole foods, such as fruits, vegetables, lean proteins, and whole grains. A shift away from a Western diet high in refined sugars and saturated fats towards a diet incorporating DASH or Mediterranean elements can amplify the health benefits. For instance, foods high in beta-glucan, like barley and oats, can help in maintaining good health. Balancing macronutrients and ensuring you’re not in a significant caloric intake surplus is important, even when within your eating window.
Physical Activity and Exercise Interplay
Integrating exercise into your lifestyle while on an intermittent fasting regimen is beneficial and can enhance the overall health advantages. Exercise typically complements fasting by promoting better health markers including, cardiovascular health and insulin sensitivity. It’s about finding the right balance and timing that allows you to fuel your workouts effectively, possibly timing your meal to be before your exercise session for energy, or after to ensure recovery. Regular physical activity should be a key aspect of your lifestyle, whether you choose to partake in it during your fasting period or within your eating window.
Factors Influencing the Effects of Intermittent Fasting
When considering intermittent fasting for your gut microbiome, it’s important to understand that the effects can vary widely due to several factors. From genetic makeup to your environment, and even your medication use, these elements can influence how your body responds to fasting.
Individual Variability in Response
Your individual response to intermittent fasting is shaped by genetic factors that are unique to you. Genetic makeup, for instance, can determine the speed of your metabolism and how your body reacts to periods without food. This directly affects the changes that take place in your gut microbiome during fasting.
Environmental and Seasonal Influences
Environmental factors and seasonal variation can also play a role. The time of sunset and sunrise varies with the seasons and may impact your eating patterns and, consequently, the fasting period. Your dietary choices, potentially influenced by available seasonal foods, can modify the gut microbiome’s composition during fasting.
Medication and Antibiotic Use
Medication and antibiotics can significantly affect your gut microbiota. While you fast, any medication you take may interact differently with your body compared to when you are consuming regular meals, which could alter the fasting’s effects on your gut bacteria. Furthermore, antibiotics are known to disrupt the balance of gut microbiota, which might counteract the benefits of intermittent fasting.
Future Directions and Concluding Thoughts
The frontier of research into intermittent fasting and the gut microbiome is poised to enhance your understanding of human health. Here, the latest trends in research and the potential for disease prevention are detailed, alongside important ethical considerations.
Emerging Trends in Intermittent Fasting and Microbiota Research
Recent findings suggest that intermittent fasting can lead to a significant abundance of beneficial gut microbes. These findings hold promise for future studies that aim to decipher the complex relationships between dietary patterns and microbial composition. Specific areas of interest include the impact on metabolic disorders like obesity and type-2 diabetes, as well as cancer and cardiovascular disease.
Potential Applications for Disease Prevention and Management
Excitingly, the manipulation of gut microbiota composition through dietary interventions such as intermittent fasting may offer new ways to manage and possibly prevent conditions like inflammatory bowel disease. With emerging evidence supporting the role of gut health in systemic diseases, you can expect a surge in personalised nutrition plans that utilise fasting as a tool for public health optimisation.
Ethical Considerations and Public Health Implications
When integrating intermittent fasting into public health recommendations, it’s essential to consider ethical considerations. Ensuring equitable access to accurate information and dietary interventions across different populations is crucial. Moreover, future research must balance enthusiasm with rigorous testing to avoid the premature elevation of fasting regimes to clinical practice without conclusive evidence.
Frequently Asked Questions
Intermittent fasting can significantly affect your gut microflora, with research suggesting changes in microbial diversity and function.
How does intermittent fasting influence gut microbiome diversity?
Intermittent fasting can reshape your gut microbiota, with studies indicating variations in microbial diversity due to different fasting durations.
Can a 24-hour fast improve gut health?
A 24-hour fast may have an impact on your gut microbiome, although the specific effects can vary from person to person. Some evidence suggests short-term fasting might promote gut health.
Is there evidence that intermittent fasting can reduce gut inflammation?
Intermittent fasting has been associated with a reduction in gut inflammation, as fasting can influence the composition and function of the gut microbiota.
What are the effects of a 48-hour fast on the gut microbiota?
A 48-hour fast can lead to noticeable changes in gut microbiota composition and is thought to be connected to several health benefits.
Could long-term fasting have a beneficial impact on gut microbiota?
Long-term intermittent fasting could potentially enhance gut microbiota diversity and contribute to better metabolic health, but the long-term effects warrant careful investigation.
Are there any negative effects of fasting on beneficial gut bacteria?
While fasting may have benefits, prolonged fasting could also possibly disrupt the balance of beneficial gut bacteria, highlighting the importance of a personalised approach to dietary fasting regimens.
About Us
Our goal is to empower you with concise probiotic guidance for a healthier gut. With expert advice, we provide the knowledge to improve your well-being and navigate the world of probiotics efficiently, ensuring you achieve optimal gut health.
- Can You Take Probiotics While Water Fasting?
- Does Fasting Help Microbiome Diversity and Functionality?
- Does Fasting Help Your Bowels
- Does Fasting Help Probiotics? Understanding Gut Health Benefits
- Does Fasting Help the Gut: Understanding the Impact on Digestive Health
Disclaimer
As an affiliate, we may earn a commission from qualifying purchases. We get commissions for purchases made through links on this website from Amazon and other third parties.
Check these out on Amazon








